America, Inflamed

Here is a modernist myth that often gets people into trouble: problems have simple causes.
You see this idea everywhere, from the diagnoses of our sclerotic body politic (disinformation!) to the decades-long refusal of world leaders to grapple with the threat of climate change (human nature!).
For a graphic example of this, Politico ran a story last week that argued that the perpetual staccato of government near shutdowns — sparked, time and time again, by revanchists on the hard right Freedom Caucus in the house of representatives — might actually be a result of the introduction of air conditioning, which (the piece claimed) had allowed the congressional season to push so far into summer recess as to make last minute debates into metastatic, process-disrupting obstacles.
It's not that these causes aren't necessarily valid, so much as that they subscribe to a seductively simple view of the world. One in which the clean narrative line of the police procedural superimposes upon the messy and entangled reality — a "one weird trick"-ification of life into a series of Sherlock Holmes stories with a nice pat conclusion at the end.
Would that it were so simple.
Welcome to Heat Death, the newsletter that embraces the deep, difficult tangle of cause and effect. A spate of rain has finally penetrated the Austin heat dome, bringing a touch of green and marginally cooler temperatures to the baking landscape. Asher has been crisscrossing the state, visiting fossil exposures and the vaults of natural history museums. (He found time to cover the re-opening of Austin's Texas Museum of Science and Natural History, but a sneak peak of what all of this is in service of will have to wait.) Saul, meanwhile, has been dug in right here at home, balancing his duties at The Hill with the raising of the wee baby Max.
But enough about us. We're thrilled to welcome back to anthropologist and Heat Death contributor Annika Tara, who last graced us with a great essay about sexgender, biological determinism, and the false promise of safety in taxonomy. Annika's been giving a great deal of thought lately to the problem outlined above: the desire for simple answers to extremely complex questions. As Annika writes in today's dispatch, nowhere is this tendency more pronounced or pernicious than it is in medicine: a domain where we are still shackled by the long intellectual history that involves thinking of the body as a machine, and its disorders as mechanical breakdowns.
In a wide-ranging essay, Annika lays out some conclusions suggested by ongoing research: that the strange and phantom diseases that currently stalk us arise from strange interactions within our bodies, physical forms that have spent lifetimes marinating in the terrible chemical soup of modern America. And Annika's ready to give that system a name.
It's Heat Death, everybody. Stay with us.
Welcome to the Inflammatory Industrial Complex
Annika here. America is sick.
That’s not a metaphor. I mean it literally: people in America are ill. Despite the extraordinary price tag of our healthcare, we suffer from more diseases than people in comparable countries. We die younger and sicker.
Sure, we may have managed to tame the most virulent killers of centuries past. But chronic, noncommunicable diseases? Conditions of slow breakdown and accumulating dysfunction? These we have in spades.
There are the bog-standard maladies that dog most of our elder years, like heart disease, diabetes, and cancer. Then there are the common but poorly understood chronic conditions: hot-girl-afflicting IBS (and its nastier cousins, IDB and Crohn’s disease), polycystic ovary syndrome and endometriosis, fatiguing diseases like myalgic encephalomyelitis, chronic pain disorders, complicated allergies and intolerances.
And there are the people who — despite lacking a formal medical diagnosis — just feel like garbage all the time: run down, haunted by aches, pains and mysterious digestive issues, somehow both perpetually tired and too wired to sleep well. The postindustrial walking dead. Maybe you’ve heard their complaints echoing through the break room or the halls of cyberspace. Maybe you’re one of them.
Lately, the problem of chronic disease has increasingly edged its way into the limelight. Bestselling memoirs detail the vagaries of life with complex, poorly understood chronic diseases. Podcasts and documentaries ruminate on medical mysteries. And over the past three years, Long COVID patients and advocates have drawn attention to the challenges that people living with such conditions face — and just how poorly equipped our society is to respond to them.
All of this chafes against how we're taught to think about the march of modern, Western medicine. As school kids, most Americans are taught a casually triumphal version of medical history. According to that account, we vanquished most major diseases over the course of the late 19th and early 20th centuries, through the discovery of bacteria, and thus improved sanitation practices, vaccines, and eventually antibiotics. In this story, diseases that prevail now are essentially leftovers — remnants scattered in the dust of that historic victory. Sure, there are a few tough nuts left to crack, like cancer. But by and large we’re living on the bright side of medical history.
What, then, do we make of the precipitous rise of chronic diseases in the U.S.? The triumphal narrative brushes them aside. Mostly, we are told, the chronic diseases of the 21st century are a perverse result of medical progress: only recently have enough people begun living long enough for the diseases of aging, or the kind of inherited conditions that might have led to early death in the past, to become significant at the population scale. Otherwise, modern chronic diseases are cast as problems of “lifestyle,” attributable to our decadent diets and (lack of) exercise habits.
While I’m as thrilled as anyone not to have died of measles as a toddler, there’s a lot missing from this story. Fixating on individual choices and life trajectories keeps us from asking bigger questions about the conditions that allow the cornucopia of chronic diseases to thrive.
Since 2016, I’ve been studying how people who live with complex chronic diseases get by in a medical system and a society that wasn’t built for them. I’ve interviewed patients, observed and participated in forums and support groups, attended conferences and advocacy events, and pored over medical studies.
Through this work, I’ve learned about a different way of thinking about disease that helps to explain:
- why chronic disease is so prevalent in the U.S.
- why it’s so hard for patients to access meaningfully helpful treatment, and maybe even
- why so many of us are schlepping around feeling like garbage all the time, whether we have a formal medical diagnosis or not.
There’s a lot to unpack here, but to put it as succinctly as possible: It's not your fault.
Let me repeat that: It’s not your lifestyle. You didn’t do it to yourself. It’s not your crappy genes, either.
It’s something much bigger than that. The real drivers of 21st century chronic diseases are literally and figuratively in the air that we breathe.
I’ve been calling this phenomenon the inflammatory industrial complex: a tangle of social, economic, and infrastructural forces that demands most of us endure near-constant exposure to toxic substances, infectious diseases, and inescapable stress. The result is a slow, compounding death-by-a-thousand-cuts.
For the fortunate among us, it manifests as the constant headache, the finicky stomach, the mercurial malaise. But in the worst cases, it can result in a debilitating downward spiral of multisystemic disease, leaving people stranded on the margins of medicine, sick in ways that we don’t have words for.
But before embarking on our grand tour of the inflammatory industrial complex, it’s worth taking a moment to examine some of our ideas about what a disease is, and how we imagine them to work.
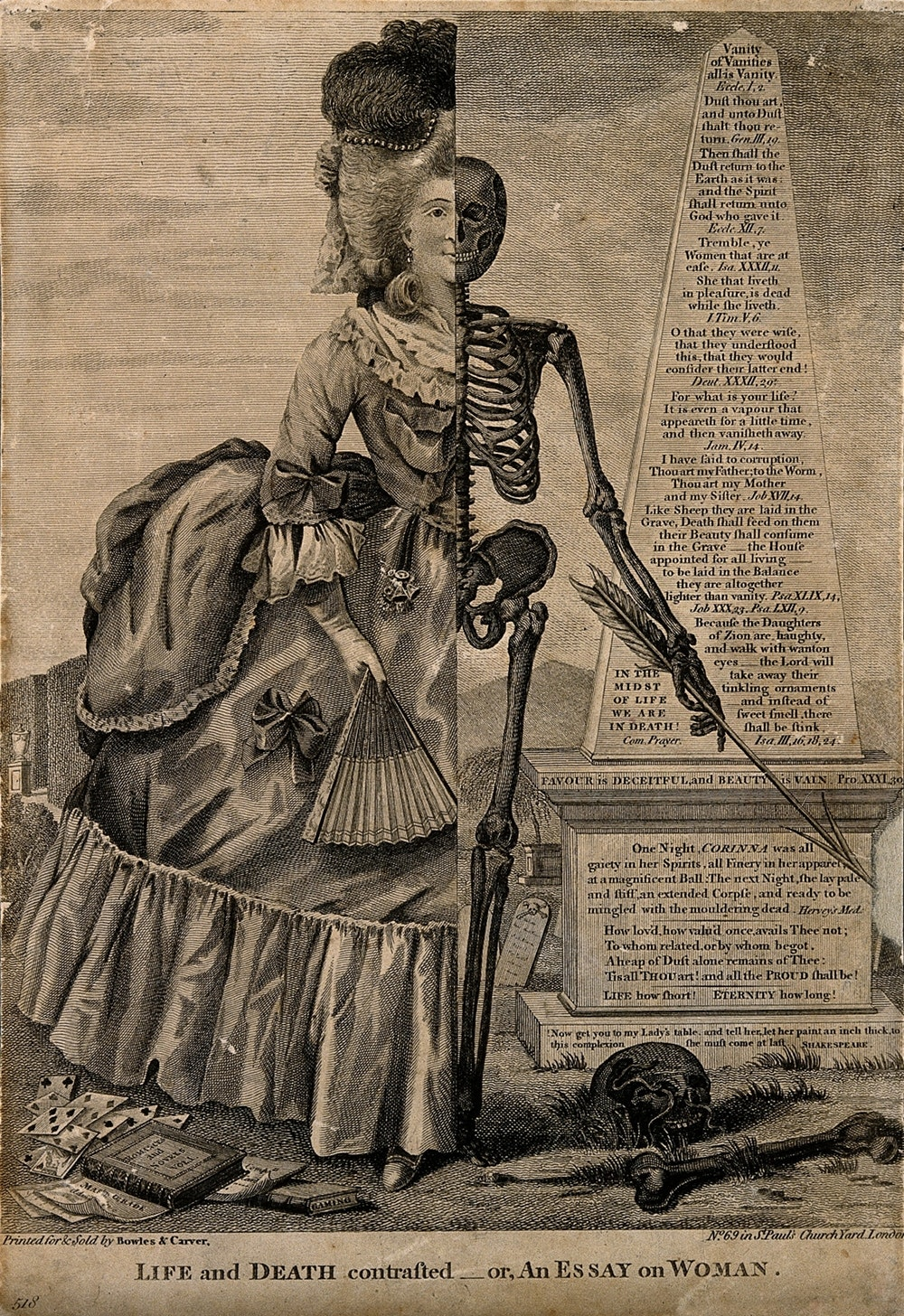
Modern Americans tend to think of bodies sort of like machines made up of so many moving parts —and, consequently, of diseases as the kind of mechanical dysfunction that might cause a machine to break.
In this schema, that breakage gets conceived as singular and localized. It follows from this idea that diseases are unique and discrete: every disease has a unique mechanical identity (that is, the thing that’s broken) that distinguishes it from all other diseases and explains its effects. If you look around, this idea is everywhere.
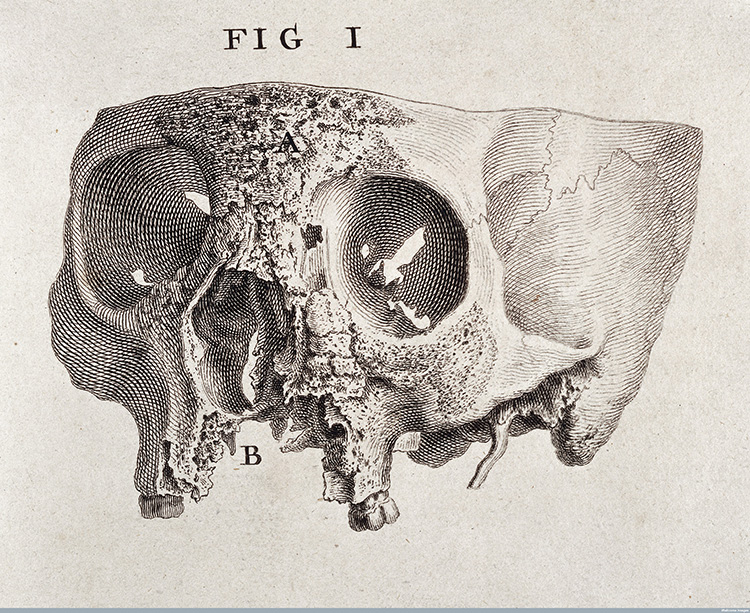
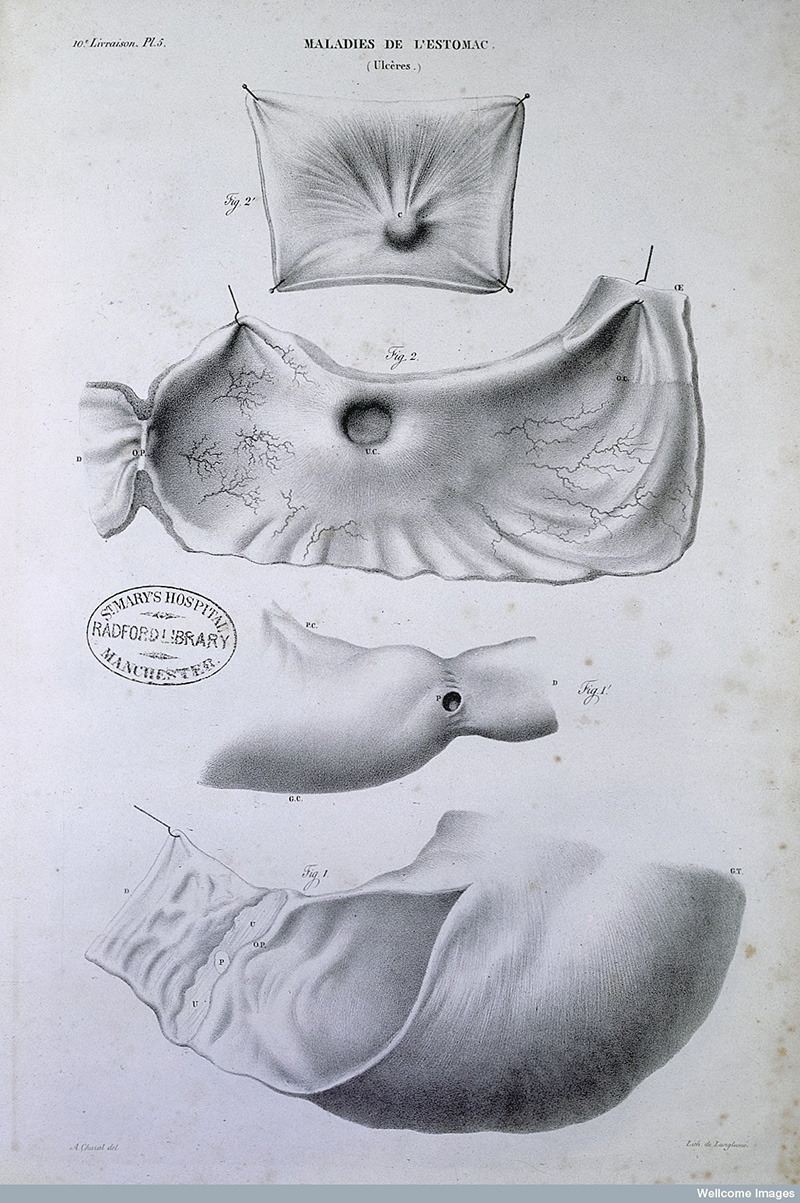
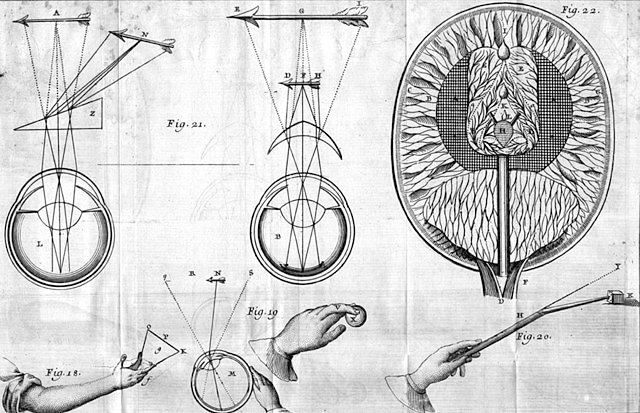
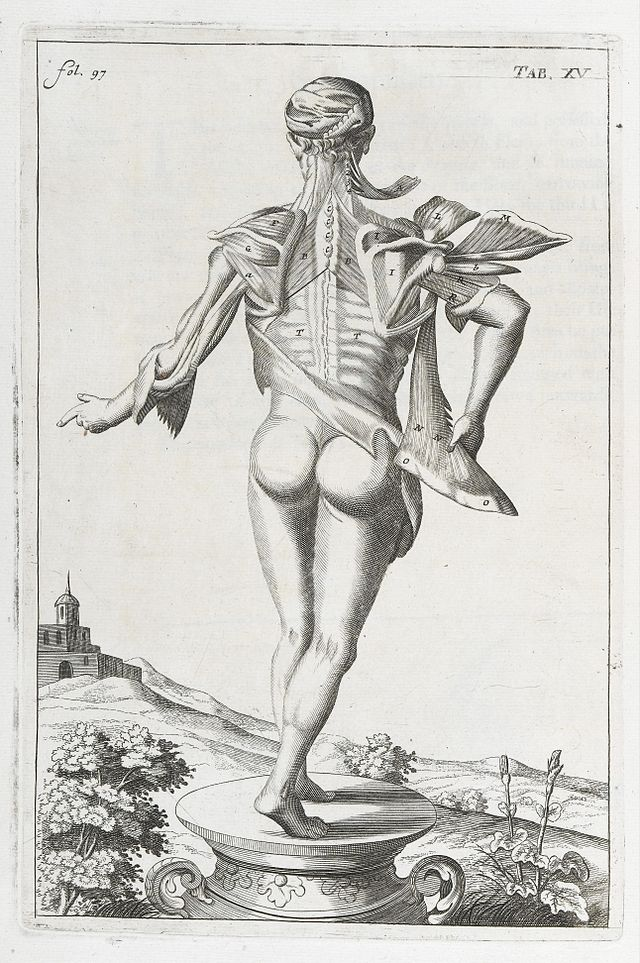
There's nothing essential about this idea. Like all ideas, it came about in a specific historical, cultural, and technological context. Historians of science locate the emergence of this “disease as discrete dysfunction” theory somewhere between two separate events. The first was the embrace of human dissection as a scientific practice. For much of the European medieval period, human dissection was relatively rare (as a result of religious taboos), and surviving records of ancient dissections were few and far between. But as social moores began to change, dissection reentered scientific practice. Opening up the human body allowed scholars to literally see our organs as a collection of separable parts, like the gears in a clock.
The other factor in the emergence of disease-as-mechanical breakdown was the emergence of germ theory in the early modern period, and then the modern sanitation practices, vaccines, and antibiotics that followed, all of which reshaped our collective relationship with infectious diseases.
And fair enough. If we take infectious diseases as they were known in the mid-20th century, at the height of the antibiotic revolution, as a model for sickness in general, the “disease as discrete dysfunction” idea makes a lot of sense. If it turns out that all of the symptoms of, say, tuberculosis, can be traced to the presence of a bacteria and wiped out with a drug that’s like a silver bullet, why couldn’t the same be true of other diseases? This kind of logic continues to drive a great deal of research and drug development today. It’s the basic idea behind the serotonin deficiency theory of depression, for instance. Does your brain not produce enough “happy chemicals”? A selective serotonin reuptake inhibitor (SSRI) can fix that.
Except it might not be nearly so simple. Sticking with mental health: recent meta-analyses of research on depression have cast serious doubt on the serotonin deficiency theory. The simple mechanical fix, in other words, doesn’t work.
And if we zoom out, we notice that the same is true of most of the chronic diseases of the 21st century. There are no miracle drugs that can cure diabetes, or autoimmune disease, or neurodegenerative diseases.
Instead, I want to suggest that diseases like these demand a new way of thinking about sickness. And once we shift our perspective away from the idea that all diseases can be traced to a single source and fixed with just the right targeted tweak, the whole fusillade of harms perpetrated by the inflammatory industrial complex comes into focus.
Why? Because unlike the parts in a car or the gears in a clock, our crucial body functions aren’t meaningfully separate from another. You can’t always isolate a disease to one organ or type of tissue or cell, because organs, tissues, and cells are in constant interchange with each other. Our bodies are systems made of systems - interlocking and overlapping processes that are always in motion, responding to both one another and our environments.
One of those systems-within-systems is the immune system, the origin of inflammation: the health buzzword of the moment. (In fact, if I was in the business of making predictions, I might even say that “inflammation” is poised to become the next “trauma” - the all-purpose malady of the moment.)
Given that, it’s helpful to remind ourselves that inflammation isn’t inherently a bad thing. Inflammation is a catch-all name for a set of processes that occur when our immune systems respond to distress signals from infected, damaged, or aging cells. The heat and swelling around a cut, the fever and aches that come with the flu —- that’s inflammation. Without it, we wouldn’t be able to heal injuries or fight off infections.
A healthy inflammatory response is powerful, but that also makes it a little dangerous. (Like many biological processes, inflammation is a Goldilocks quantity: too little is just as harmful as too much.) The big problem, here, isn’t that inflammation exists. It’s that we’re living under conditions that are making it harder and harder for our bodies to regulate the inflammatory response -- to keep it in its lane, so to speak. And as we’ll see, a whole host of other problems can accompany inflammation when it becomes dysregulated.
The immune system works in close concert with the nervous and endocrine systems. All three are distributed throughout our entire bodies, produced across half a dozen different organs and made up of scores of specialized cell types. All three share a common cohort of molecular “messengers” enabling them to communicate with and mutually regulate one another. Anatomy textbooks assign these to one system or another — neurotransmitters to the nervous system, hormones to the endocrine system — but in practice, there’s a lot of cross-talk.
Much of that conversation happens in our digestive system. Until fairly recently, we in the West have considered the brain the “control center” of the human organism — the intelligent hub that animates the rest of our bodies as though they were (as the phrase goes) meat puppets. But it turns out our digestive systems are an enormous hub of activity, and what goes on in our guts plays a huge role in our overall health. The coils of our intestines are home to some seventy percent of the total immune cells in our bodies, as well as a flurry of neurotransmitters, including ninety percent of our serotonin. There’s so much going on in our guts that some researchers have begun to understand the stomach and intestines as a second brain.
The digestive tract is also home to the millions of organisms that make up our microbiomes. Throughout our entire lives, interactions between microbiome bacteria and immune cells affect how we respond to disease, injury, and novel environments. Because communication between the central nervous system (the brain and spinal cord) and the enteric (digestive) nervous system runs both ways, microbiome health might even impact our moods and conscious experiences. Although the causal direction of these relationships hasn’t yet been established, studies have associated mental health and neurological conditions including depression and Alzheimer’s disease with altered microbiomes.
Rather than acting like different parts in a machine, the digestive, nervous, endocrine, and immune systems are closely interconnected, both spatially — they literally overlap in our blood and tissues — and functionally. They work because they work together.
Take the famous “fight or flight” response as an example. When our brains perceive something dangerous or threatening, they stimulate the adrenal glands to release adrenaline and cortisol. These, in turn, kick the autonomic nervous system into high gear: heart rate and blood pressure rise, lungs take in more oxygen, alertness increases, and circulating blood sugar rises, providing a burst of energy.
“Fight or flight,” in other words, is an adaptive nervous system response that helps prepare us to deal with potentially hazardous situations. But it's not just a nervous response. Those other body systems – endocrine, immune, and digestive – are also involved. The changes in autonomic nervous system activity that affect heart rate and respiration are mediated by hormones, which are themselves produced by the several organs that belong to the endocrine system. In the throes of an adrenaline rush, our digestion slows down and some immune activity becomes inhibited — perhaps to redirect resources away from those energy-intensive processes and towards fighting or fleeing. In fact, the physiological “opposite” of the fight or flight state primes us for just those two activities — it’s commonly called “rest and digest.” (Or, in a phrase that could have been cribbed from a fetish site, “feed and breed.”)
Both the fight or flight response and inflammation are a normal part of being in a body, and they illustrate well how the nervous, immune, and endocrine systems can work harmoniously. But with chronic disease, these interconnected systems go haywire.
To illustrate this, let’s look at a lecture by Dr. Andrew J. Maxwell, a cardiologist, at a 2019 conference. Maxwell discusses his hypothesis about the disease process underlying a cluster of five frequently co-occurring conditions that he calls “the pentad.”
The initial element of the pentad, Ehlers Danlos syndrome, makes collagen — a structural protein —weaker than it should be. Collagen is a key ingredient in the connective tissues that hold joints, organs, nerves, and blood vessels in place as we move around. Weak collagen can cause these support structures to shift or sag. In the right (or wrong) place, this can result in compressed blood vessels and nerves, which in turn can affect blood pressure and heart rate.
At first, these symptoms might be very mild — maybe not even significant enough to register as unusual for the person experiencing them. But they can worsen over time — paradoxically, as a result of the body’s attempt to compensate for them.
Here’s Maxwell’s hypothetical example of what that can look like. First, low blood pressure leads to fluid pooling in the lower half of the body, because there isn’t enough pressure to push it upwards against gravity. Then the kidneys —located in the lower abdomen behind the stomach — misinterpret the relative abundance of blood as overhydration, so they increase urine production in order to rid the body of the “excess” fluid. The increased drain-off, in turn, makes it harder for the heart and blood vessels to maintain normal pressure. Over time, the body tries to compensate for low blood pressure and a slow heart rate by increasing adrenaline and cortisol to boost them. But — as we’ve seen in the fight-or-flight response — this, in turn, has cascading effects on the immune and digestive systems.
For some, the spiral might stop here. Impaired blood pressure and heart function might make it difficult to adapt to the demands of physical activity, or cause lightheadedness or even fainting (as in dysautonomia, the second element of the pentad.) Elevated stress hormones may make it difficult to sleep (that familiar “wired but tired” feeling — the affect of the moment), which itself has a whole host of downstream effects.
For many, this kind of ailment lives somewhere in the no man’s land between health and full-blown disease. It definitely doesn’t feel good. It can even be disabling. But if a person at this stage of neuro-immune-endocrine dysfunction were to seek medical treatment, the odds would be stacked against them. The more dramatic symptoms of autonomic nervous system dysfunction can be fickle, and if they don’t happen to show up during a ten minute scheduled medical appointment, the most readily measurable signs —like low blood pressure —are unlikely to cause much alarm on their own. If a doctor doesn’t conjure them so they can be observed and measured (say, with a tilt table test), or isn’t willing to pursue further testing, the patient is back to square one. Add to this an economy where time and money are tight and a culture that valorizes powering through sickness and discomfort, and meaningful medical treatment starts to look like a mirage on the horizon.
Meanwhile, the cascade continues. Let’s keep tracing Maxwell’s pathway of breakdown. Stalled digestion from elevated stress hormones leads to changes in intestinal pH levels, which in turn alters the makeup of the gut microbiome. This might manifest as gastrointestinal symptoms, like slowed or painful digestion (gastroparesis: pentad component number three). As internal ecology goes out of whack, so too do the immune activities that depend on gut microbes. At the same time, consistently elevated adrenaline and cortisol levels can suppress immune activities in their own right.
All of this creates conditions of increased susceptibility to infectious disease, which (as we’ll learn more about shortly) can knock the neuro-immune-endocrine supersystem even further off its axis. Over time, a stressed immune system might start making mistakes - like setting the cells meant to kill bacteria and viruses against ordinary, healthy tissues (autoimmune disease: pentad component number four) or going haywire with allergic reactions (mast cell activation syndrome - completing the pentad).
Thus, Maxwell argues, what might initially look like five different disorders that happen to pile up on one unlucky person actually turns out to be a single pathological process, unfolding over time across many body systems, in response to both external stimuli and internal ones: a spiral that, once triggered, feeds on itself.
That bodies are always responding to their environments is a commonplace observation. But its implications don’t stop at the skin: the immune, nervous, endocrine, and digestive systems effectively are one anothers’ environments. Because they’re so closely interconnected, an injury or defect in one of these systems can have cascading effects in the others.
Think of it like choreography. To a large extent, our system-of-systems is intelligent and self-correcting: it can modulate the way that life-sustaining processes (including inflammation) unfold in order to adapt to changes, and very often it can compensate for a little bit of damage here and there. It’s a lot like the way a group of highly trained and well-practiced dancers can work around a single stumble or misstep — maybe even so seamlessly that the audience doesn’t notice.
But if disruptions keep happening — if one person is persistently off-beat, or if several people make mistakes at the same time — it becomes increasingly difficult to maintain the integrity of the dance.
I’d be remiss if I didn’t acknowledge that this way of thinking isn’t exactly mainstream within medicine. There are those who argue against this interpretation - but personally, I’ve yet to find them especially convincing. Some detractors simply assert that there’s no evidence for these kinds of disorder(ed) interactions. But even a quick PubMed search suggests that this isn’t the case. Yes: there are plenty of unanswered questions. At this stage, there are more questions than answers, given the sheer number of cell [types] and [messenger] molecules at play in neuro-immune-endocrine interactions. But there are also plenty of thoughtful hypotheses that warrant serious consideration, like the one I’ve described here.
The other naysaying tactic is to question whether diseases like MCAS and POTS — components of Maxwell’s pentad — actually exist as distinct maladies, usually on the ground that their symptoms are too “vague” to point any singular dysfunction. I find this equally unsatisfying, since many diseases are “vague” at the level of symptoms. A fever with cough and head and body aches could signal any one of a dozen different viral or bacterial infections, but absent a patient history and further diagnostic testing, we may never know which one. That doesn’t mean we dismiss the flu or strep throat as vague. Likewise, autoimmune diseases can be difficult to diagnose and categorize due to their wide array of potential symptoms and temporally fluctuating, relapsing-and-remitting nature. Lupus and MS have both been called “great imitators” for the frequency with which they’ve been mistaken for other conditions. That doesn’t mean we should write off the category of autoimmune disease entirely.
But this system-of-systems way of thinking does make it more difficult to conceptualize ill health as something whose varieties we can sort into in neat, separate boxes. When you carve nature at its joints, so to speak, you’re also cutting through a whole lot of tissue and blood vessels and disrupting processes that, in vivo, operate across the whole organism.
Though Maxwell presents his theory of the pentad in narrative form, moving from one disorder to another, cumulative, multisystemic illness won’t always follow the pattern he lays out. Instead of a disorder like Ehlers-Danlos syndrome, the inciting factor could be an injury that damages nerves. Or the spiral might begin with an infectious disease. The sheer number of variables involved — the dozens of processes and functions governed by the hundreds of cells and messengers that make up the neuro-immune-endocrine system, any of which can be damaged or thrown off-balance — means that the path from initial illness to severe chronic impairment might look a little bit different for everyone.
This kind of idiosyncrasy is at odds with both medical orthodoxy and the U.S. health care system’s love affair with bureaucracy. Between understaffing, drug shortages, and the vagaries of institutional management, our health systems can barely handle the most straightforward of medical problems. They were not built to handle the kind of detailed, trial-and-error investigation that it takes to make sense of a multisystemic disorder of process —much less to slowly nudge the pieces towards a healthier state when every intervention could have cascading effects that impact the whole system.
Faced with these kinds of “vague” diseases, many clinicians will simply shrug their shoulders and shuttle patients along through an exhausting and expensive gauntlet of specialist referrals. Or they’ll chalk it up to a “lifestyle” problem like stress or weight. Doctors who are willing to investigate often require payment in cash, because few insurance plans are likely to approve extensive exploratory testing, or intervention without a diagnosis that meets established standards.
This leaves people living with these diseases in a kind of limbo, sick in a way that doesn’t fit into the blanks on the form. And this is not an accident. Enter the inflammatory industrial complex.
I want to be very clear here: I’m not espousing a conspiracy theory. Unlike the “plandemic” crowd, I don’t claim that there’s some all-powerful cabal out there that wants us to be sick. In a way, it's worse than that. The ways we live, work, and consume — not to mention our whole political reality — are literally poisoning us.
This isn’t by anyone’s particular design, but it doesn’t need to be. To the people who profit from the industries that make up the inflammatory industrial complex, epidemic chronic disease is just an unfortunate side effect of massive financial success. And if that can be swept under the rug by blaming those diseases on “lifestyle” choices and inborn faulty genes — that saves everyone from having to ask some inconvenient and expensive questions.
So it’s time to meet the monster: the three-headed dragon stoking the fires of chronic disease in America.
First, there are infectious diseases.
Let’s start with the big one: COVID-19. Although the Biden administration declared an official end to the emergency and the CDC has dramatically scaled back its monitoring of transmission data, the COVID-19 pandemic is ongoing. Even if it weren’t, it would still loom large in the sheer number of people affected: by the end of 2022, almost three quarters of Americans had contracted the virus, according to a CDC estimate. For an unknown number of people, the impacts of the virus linger. In emerging research, COVID-19 infection (even with only mild symptoms) has been associated with damage to the heart, vasculature, lungs, kidneys, brain, and immune system.
Patient organizing around Long Covid has prompted the medical establishment to ask bigger questions about the long-term consequences of infectious disease. But COVID-19 is far from the first infectious disease to be associated with long-term symptoms. Ebola, Epstein-Barr virus, Dengue fever, Q fever, chikungunya virus, polio, West Nile virus, and at least two human herpesviruses have all been linked to chronic disease post-infection.
How do acute infections cause long-term illness? Research points to multiple potential mechanisms. In some cases, the virus or bacteria itself may linger in our cells and tissues: even small fragments of a virus — like the spike protein that coats the outside of the COVID-19 virus — can provoke ongoing immune response after the acute infection has apparently resolved. There’s some evidence that lingering infections can spring back to life if their host’s immune system becomes compromised — such as by contracting another disease, resulting in a “superinfection.”
The precise ways that concurrent infections interact is also an open question. Evidence from hospitalized COVID-19 patients suggests that the presence of reactivated Epstein-Barr virus heightens risk of pneumonia and mortality. Infections can also cause direct damage to organs and tissues that persists well past the acute infection, causing a kaleidoscope of potential problems depending on where the damage accumulates.
In other words, evidence is mounting that in many cases, infectious diseases are not simply “cleared” from our bodies, leaving them exactly the same as they were before. Every encounter with a disease has the potential to leave a trace, whether subtle or dramatic, that could affect how we respond to other diseases or stressors in the future.
We’ve seen over the past three years just how ill-equipped the U.S. is to manage novel infectious diseases. And that should be cause for concern, because the future likely holds more of them.
Consider the matter of zoonosis: the transmission of disease from animals to humans. The term entered the popular lexicon in 2020, unfortunately often attached to anti-Chinese stereotypes and vague, sinister terms like “wet market” (which actually refers to a market that sells fresh produce and meats, like a farmer’s market). While COVID-19 most likely did come to us from animals, the problem has little to do with the exotic eating habits of foreigners. Around the world, habitat destruction for the sake of resource extraction and development has forced animals into much closer proximity with both each other and humans, increasing the likelihood of the kind of close encounters during which disease can jump from one species to another. On top of this, climate change means that many “tropical” vector-borne diseases are showing up in locales farther removed from their historical hot spots. (Dengue fever in Florida, anyone?)
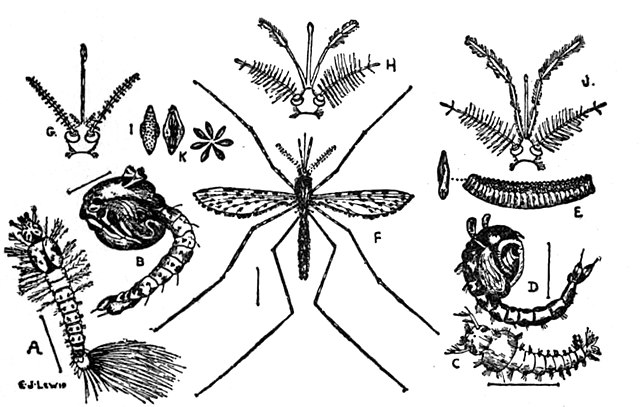
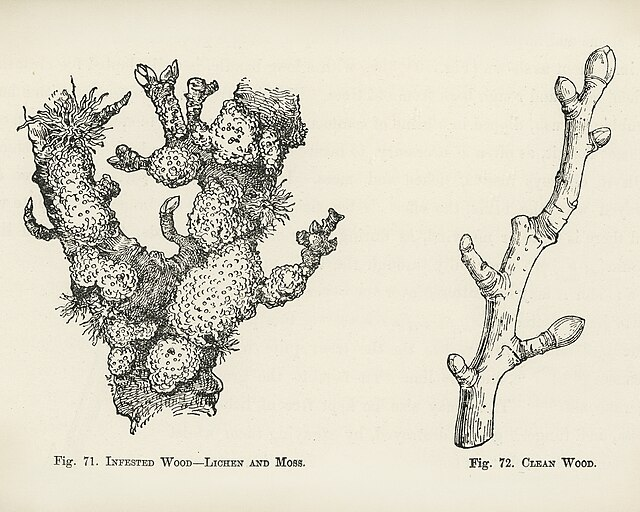
Risk of zoonosis isn’t confined to far-off forests and jungles. It’s in our back yards, too. As suburban sprawl in the U.S. encroaches on wooded habitats, tick-borne illnesses like Lyme disease have become more common. We also have our massive meat, egg, and dairy industries to worry about. Disease transmission among animals living together has always posed a problem for farmers. In the mid-20th century, however, large scale animal farming operations started dosing their livestock with prophylactic antibiotics to prevent infections from running rampant in increasingly crowded facilities. Decades on, factory farms face the same challenge that many hospitals face: bacteria with an evolved resistance to antibiotics. With hundreds of workers and thousands of animals sharing close quarters, large meat and dairy operations are effectively zoonosis time bombs.
And then there are parasites! U.S. residents tend to think of them as a tropical malady, or one confined to “Third World” countries that lack modern sanitation infrastructure. But recent research suggests that parasites are thriving in U.S. populations, too — especially in under-resourced communities. Parasites stay alive inside their hosts by evading our immune systems, but they exact a toll on our bodies in other ways. They can absorb nutrients before their host is able to, leading to malnutrition. They can also cause damage to the particular type of cell or tissue they inhabit: the malaria parasite, for example, causes anemia by impairing and eventually destroying the red blood cells it infects. And, as we now know, any such damage could have downstream effects as other body systems attempt to compensate for it.
Many parasitic infections are, in theory, easy to treat with anti-parasitic drugs that either kill the organism or prevent it from reproducing. But in the U.S., runaway drug prices mean that even decades-old, bog-standard antiparasitics can cost hundreds or thousands of dollars. And beyond that, if the conditions that lead to infection — like contaminated drinking water — aren’t remedied, reinfection is likely.
In the race to sweep the pandemic into the dustbin of history, pundits have tried to position infectious disease as a normal and natural part of life, one that poses few risks to healthy people.
In another world, there might be some truth to this. But it’s hard to argue that we in the U.S. should consider ourselves “healthy.” As we now know, our response to infection is conditioned by the whole gut-mediated neuro-immune-endocrine supersystem. For those of us living in the (bloated, sluggish) belly of the beast, the cumulative burdens of the inflammatory industrial complex may well override the protective potential of infection.
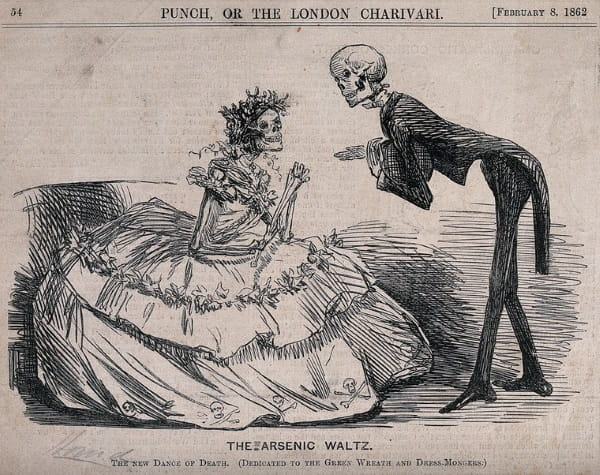
Which brings us to the second head of the inflammatory hydra: our everyday world is saturated with harmful substances. The list is long: fertilizers and pesticides that linger on unwashed produce and run off of farms and into water supplies. Air pollution caused by fossil fuels and forest fires. The truly innumerable — and largely unregulated — novel substances used in various industrial and manufacturing processes. Additives in processed foods, cosmetics, and other consumer products. Solvents and detergents in cleaning products. Heavy metals leaching from aging plumbing into our drinking water. Omnipresent plastics shedding microparticles. A 2020 estimate published in Environmental Science and Technology suggests that there are over 350,000 chemicals and compounds currently in use. The list is growing every day, and most will never be rigorously tested for safety — especially in the U.S., where privatization and deregulation rule the day.
Since at least the 1960s, people from affected communities (who are often poor, Black, and Indigenous) and environmentalists have sounded the alarm about the effects of industrial substances on human, animal, and ecological health. As a result of their efforts, a few have been restricted or banned, such as the pesticide DDT, the subject of Rachel Carson’s 1962 clarion call Silent Spring.
But these represent a drop in the bucket compared to the hundreds of new substances that seep out of labs and refineries every year.
The existence of regulatory agencies like the FDA, EPA, and the Bureau of Consumer Protection may lead you to believe that someone’s on top of all of this, monitoring the substances we’re exposed to for safety and holding the companies that produce them to account. That may have been the idea, but in truth, most regulatory agencies are hamstrung: they lack staff and the budgets to keep up with the scale of the problem, and while their mandates are broad, their authority is limited. Research lags, and loopholes abound.
Take food additives, which have lately been cited as drivers of diet-related disease. Glance at the ingredients listed on a frozen meal or packaged snack from the average American grocery store, and you’ll likely find a bunch of extracts, gums, and emulsifiers, along with compounds whose names require a chemistry degree to decipher - like “citric acid esters of mono- and diglycerides.” Most of those additives have never been meaningfully tested for safety. One large research NGO, the Environmental Working Group, finds that 99 percent of the food additives introduced since 2000 were approved through the FDA’s “Generally Recognized As Safe” (GRAS) clause - an out that was originally intended to represent processed culinary ingredients like sugar, flour, and vinegar that have been around for hundreds of years, but which has been exploited mightily by the food industry. Effectively, the companies that make processed food additives are allowed to simply assert that they’re safe — no evidence required. Independent research has demonstrated that some ingredients approved through the GRAS loophole caused cancer in animals - which, according to the FDA’s own rules, ought to exclude them from approval for human consumption.
The same problem exists in non-food consumer products, including the packaging that food comes in. Cosmetics and personal care products — makeup, soaps, shampoos, lotions, shaving creams, fragrances, and so on — are also largely unregulated. While the FDA collects reports of adverse events in individuals and can issue warnings to consumers, there’s little they can do to stop companies from selling products or force them to change their formulas. But common cosmetic ingredients have been linked to cancers; endocrine disruption and harm to reproductive organs; and neurotoxic effects.
We hear a lot about plastics in the context of littering and environmental degradation, but there’s a good chance they’re also harmful to our health — and they’re everywhere: food packaging, water bottles, household products, childrens’ toys, even our clothes are made of plastic. Microplastics — the tiny particles shed from plastic products — have now been found in human blood, organs, placenta, and meconium (an infant’s first bowel movement - implying that we’re inundated with plastics before we’re even born). It’s easy to forget, given clever branding gestures like “vegan leather,” that plastics are derived from petrochemicals - that is, fossil fuels: a virulent source of pollution. Over time, the process of improving plastics - making them lighter, more durable, more water resistant, and cheaper - has involved dozens of chemical additives, including “forever chemicals” like PFAS. What does it mean for our health that we’re saturated, inside and out, with all of these substances? It’s not looking good.
Feeling uneasy yet? We’ve just scratched the surface. Beyond the consumer products that we use every day, there are all of the substances that are used in extraction and manufacturing. People who work at or live near industrial sites experience the worst effects. Consider Cancer Alley, a stretch of land in Southern Louisiana named for its density of petrochemical refineries — or, more accurately, for their effects on the local residents, most of whom are Black. That’s a particularly egregious example, but there are neighborhoods affected by industrial pollution across the U.S. (I’m sure you can guess who’s most likely to live in them, too.)
But even those of us fortunate enough to live farther away from industrial facilities aren’t spared. All across the country, our car dependence means that air quality in urban and suburban areas suffers badly, exacerbating chronic diseases like asthma and potentially causing others, like autoimmune (rheumatoid) arthritis, inflammatory bowel disease, and connective tissue disorder. And at the molecular scale, many industrial contaminants are extremely difficult to contain. When they’re heated or aerosolized in the course of their use, they can enter circulating air, where they’ll be swept up by weather dynamics and distributed around the world, making their way into the water and soil.
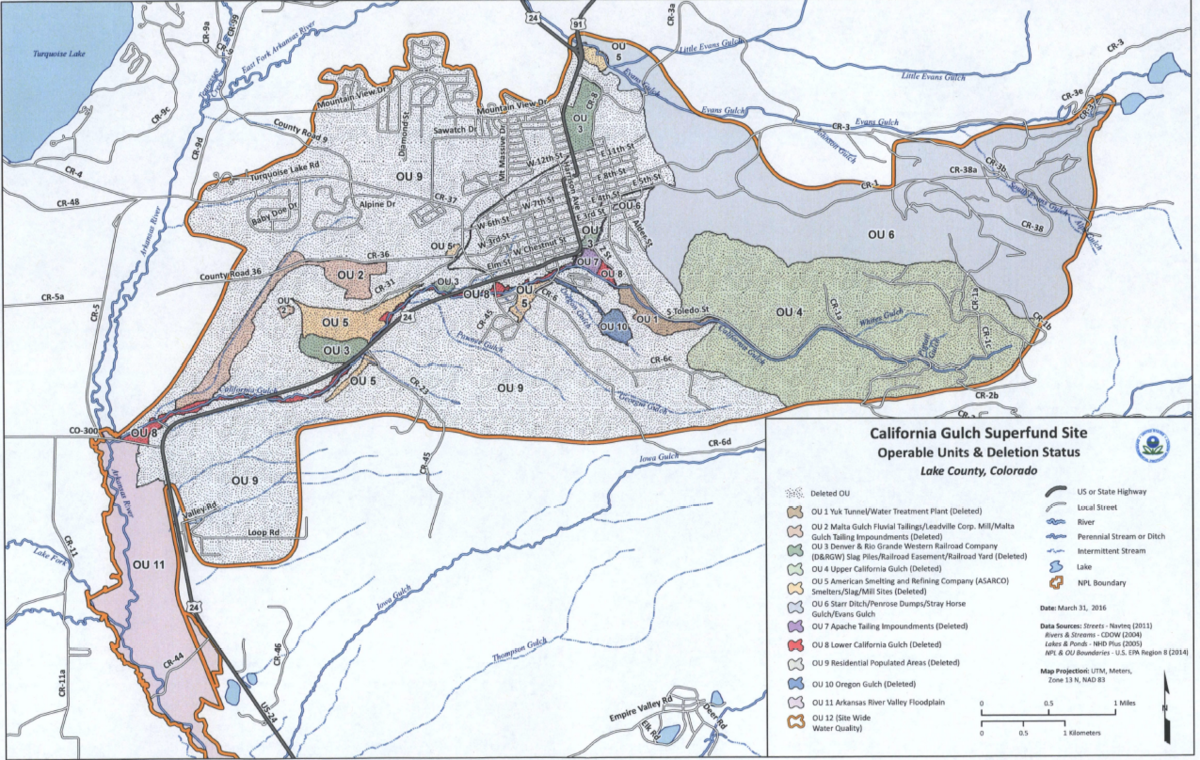
Thanks to diligent activist efforts, some egregiously harmful substances are no longer in use. But that doesn’t mean they’re gone. The U.S holds over 1,300 EPA-designated “Superfund sites,” places where industrial substances left over from past projects have been discarded and left to seep into the surrounding environment. The Superfund provisions resources for cleaning up the contamination, but progress has been slow, and people in the surrounding communities continue to feel the effects.
And then there are sources of toxicity that aren’t officially acknowledged. Scratch the surface of chemical pollution, and you’ll fall down a rabbit hole pretty quickly: hundreds of local news stories of neighborhoods that spend years suffering from unusually high incidence of chronic disease, only to find out that the vacant lot down the street where the kids play is full of polychlorinated biphenyls. That’s essentially the story of the Buffalo, New York lupus cluster, which centered on a low-income, majority Black neighborhood afflicted by multiple sources of toxicity leftover from businesses that had since closed or relocated, leaving unmarked chemical waste behind.
I want to underline that none of what I've just written is particularly controversial: autoimmune disease, neurodevelopmental disease, and endocrine system disruption — the supersystem trifecta — are all among the acknowledged effects of the industrial substances that saturate our lives. Researchers agree that a lot of the substances we come into contact with every day are harming us; this is a well-established area of concern.
Even so, I think we have good reason to believe that the situation is substantially worse than conventional wisdom lets on, because the way that pollutants are tested — when they are tested at all —doesn’t match how we encounter them in the wild.
Toxicological studies tend to test one substance at a time, and usually in single, large doses. But for most people, lived exposure is a matter of near-constant contact with dozens or hundreds of substances in tiny amounts.“The contamination of our world is not alone a matter of mass spraying [of pesticides],” Rachel Carson wrote in 1962. “Indeed for most of us this is of less importance than the innumerable small-scale exposures to which we are subjected day by day, year after year. Like the constant dripping of water that wears away the hardest stone, this birth-to-death contact with dangerous chemicals may in the end prove disastrous.”
Can many small exposures have cumulative — or mutually intensifying — effects? Great question: we’re all living the experiment. The constant day-to-day chemical bombardment of modern life is impossible to replicate in a lab environment — it’s the sort of longue-durée, multivariable process that can only be studied through a combination of basic science research and careful observation.
This has been done before: researchers figured out that smoking causes cancer through just this kind of combination of long-term observation and epidemiological reasoning. But many of us today weren’t around to witness what an epic battle it took to establish that fact against the opposition of the powerful tobacco industry.
Which brings me to the obvious next question: if all this research about the hazards of industrial substances exists, why haven’t we done more to regulate them? Some countries have. Today, regulation in the European Union follows the precautionary principle, which favors conservatism when it comes to potential health and environmental impacts. Some countries in Latin America, where peoples’ health has been dramatically impacted by predatory marketing practices on the part of large food manufacturers, now require warning labels on ultra-processed foods.
The fanatic devotion to free markets and unfettered industry in the U.S, therefore, is why I argue that the inflammatory industrial complex is an American innovation. It’s also one we’re exporting: U.S. pressure has neutered attempts at stricter regulation of harmful substances in other countries, like when Thailand tried to ban the pesticide glyphosate — manufactured by U.S.-based biotech company Bayer under the brand name Round Up — in 2019.
There’s also the matter of manufactured uncertainty, which rears its head whenever chemical industry lawyers and scientists push back against attempts at regulation. The sociologist Phil Brown, who studies health-related activism, has noted that environmental causation of illness is almost always controversial. It’s not hard to imagine why. No company or industry wants to admit that the substances essential to their success are also poisoning people, much less accept responsibility for the damages. As with the studies purporting to show that smoking cigarettes was safe, or that climate change is natural or negligible, industry-sponsored research has cleverly produced a facsimile of ambiguity around the chemical effects of their activities. (For a detailed account of how this happens, the now-classic book Merchants of Doubt remains definitive.)
To see this in action, look at the discourse about the fossil fuel extraction process known as hydraulic fracturing, or "fracking." People living near fracking sites have exhaustively documented how it ravages bodies and landscapes. Photos, videos, independent lab tests, diaries, and medical records demonstrate clear patterns of soil and water contamination, plant and animal death, and severe illness, including cancer. But according to the gas companies, this is all a coincidence, and the substances used in fracking are either “safe” or safely contained. For this to be true, the fact that a multitude of dead zones and disease clusters have fracking sites at their center would have to be a hell of a coincidence.
But this is kind of the problem: on whom should that burden of proof fall? Polluting companies get away with it in part by pointing to the multiplicity of contaminants in our environment as a source of exonerating uncertainty. You can’t hold us responsible for this, they argue, because you can’t definitively prove that any particular illness or cluster of illnesses was caused by our pollution and not someone else’s.
In some brutal way, they might be right. Who’s to say if Aunt Susan’s cancer was caused by the petrochemical refinery down the road from her retirement home, or the pesticides sprayed on the farm where she grew up, or the fumes from the dry cleaner she lived above as a young adult? It could be any of them. Or maybe it was all three, the cumulative burden adding up, over time, to more than her body could compensate for.
Our legal system, like our medical system, isn’t built to deal with these kinds of sprawling problems, where no organ or body or ecosystem or chemical or decision exists in isolation; where individual events compound one another and reality adds up to more than the sum of its parts.

There’s one last thing hammering on our collective neuro-immune-endocrine systems. In some ways, it's the most pernicious: Stress.
In 2023, stress is the medium of our lives — the water that we swim in. Life is hard. Wages are stagnant, work is demanding and dehumanizing, democracy is under attack before our eyes, and neoreactionary and straight-up nihilistic violence is so normalized that it barely makes the news anymore. Harassment, discrimination, and violence continue to terrorize people of color, immigrants, women, and queer folks. A serious illness or injury could bankrupt all but the very richest among us. The rent is too damn high. We’re drowning in debt, living paycheck to paycheck while the prices of just about everything continue to climb. You get the picture. You’re probably living it.
The idea that stress is bad for you might sound intuitive. So far, it’s been overwhelmingly confirmed by research. But it’s worth unpacking exactly how stress wears us down.
The word “stress” can be an ambiguous one. In the history of physiology and related disciplines, there’s about a hundred years of debate about whether “stress” ought to refer to the external stimuli that cause strain on our body systems, or the internal manifestations of that strain. (Or, to put it another way: is stress something we experience physically and emotionally as we rush from one job or chore or caretaking task to another, amid yet another record-breaking heat wave? Or is stress the external causes of those sensations, i.e, extreme heat itself?).
Worrying over the distinction may seem like so much scholastic prevarication, but it’ll become important shortly. In my interpretation, what’s really playing out in the competing definitions of stress is a debate about agency and responsibility: is stress something that’s foisted upon us by the world, or something that we can control by mindfulness and breathing exercises?
Stress intersects with the inflammatory industrial complex through — you guessed it! — its effects on our workhorse friend, the neuro-immune-endocrine system. Stress brings higher heart rate, blood pressure, and elevated adrenaline and cortisol. With them come all of their downstream effects, including (as we now know) sluggish immune response and digestion.
Like inflammation, stress can sometimes be helpful. In the short term, it can help us focus and muster the energy to face up to difficult tasks. In the long term, limited stress seems to be associated with greater resilience, neuroprotective effects, and improved mitochondrial function. But too much stress can be damaging. It’s a lot like athletic training: building strength and endurance involves pushing ourselves close to the edge of our current capacities — but overtraining can lead to injury, or even long-term debility. Studies have linked the concept of “toxic stress” to a “persistent inflammatory state.”
When people become so consistently stressed that they spend more time in an “up-regulated” parasympathetic nervous system state — a mode of quick responses and short term energy expenditure — than they do in a “down-regulated” sympathetic state, which prioritizes rest, cell turnover, and digestion, those crucial processes suffer. Digestion stalls out. Nutrient absorption slows down. Sleep quality suffers as circulating hormones keep hearts pounding and thoughts racing. Our ability to respond to infections suffers. (Ever been slammed with a miserable cold right after a difficult period at work, or moving house, or a breakup, or some other big life challenge? That’s probably not a coincidence.)
But the very same stress hormones that impair T- and B-cell mediated immunity (the kind that responds to specific pathogens by producing antibodies) can spur the innate immune system to action. Chronic stress can thus leave us both less able to fight off infections, and suffering the effects of runaway inflammation. Strained in both directions at once, it’s almost no surprise that the whole thing can go haywire. On its own, chronic inflammation isn’t a diagnosis or disease category. But over time, it contributes to the development of any number of widely recognized diseases, like heart disease. And it probably has a hand in the kinds of systemic neuro-immune-endocrine dysfunction that show up in clusters of connected chronic disease. You know the ones by now: autoimmune diseases, chronic digestive problems like IBS, IBD, and Crohn’s Disease, disorders of clinical fatigue like chronic fatigue syndrome/myalgic encephalomyelitis. And, of course, the wide spectrum of post-COVID effects.
Here is what the downward spiral looks like.
Maybe you’re running yourself ragged juggling work and school and you come down with a viral infection that seems ordinary — until you never get better.
Or you find yourself post-divorce and parenting alone, struggling to make ends meet, becoming more and more fatigued, until one day it’s so bad you literally can’t get out of bed — and it stays this way for years.
Or maybe you get injured in an accident, and your neck never again feels quite right despite the physical therapy. But you keep on keeping on, even as the dizzy spells, brain fog, and crushing fatigue grow steadily worse.
These aren’t hypotheticals: they are case studies, stories that I’ve heard from people who’ve participated in my research. Some of them had formal diagnoses. Some did not. But all shared symptoms that exceeded the available categories, roving throughout their bodies and changing over time in patterns that confounded many of the doctors they saw. And every one of them experienced infections, exposures, and traumas that could have caused compounding damage to their nervous, immune, and endocrine systems.
These are not spectacular stories. But that’s the point: this is how we live.
When people experiencing complex, systemic chronic illnesses seek medical attention, or try to raise broader public awareness about their suffering, they’re often dismissed with an appeal to Occam’s Razor style simplicity: they must be exaggerating, or converting emotional distress into physical symptoms. After all, if diseases are supposed to be localized, mechanical dysfunctions, then what single illness could possibly affect so many different body systems at once?
Let’s leave aside the fact that it’s perfectly possible to have more than one disease at the same time (as fully a quarter of Americans do.) Considering bodies as a dynamic systems-of-systems — rather than machines made of individual parts — suggests its own kind of simple explanation. To wit: diseases and dysfunctions of all kinds can cause systemic symptoms and change over time because our body systems aren’t isolated from one another.
In fact, we can go further. Take the appeal to simplicity and scale it up, beyond the individual. Consider what we’ve discussed about
- the toxic effects of many substances in our environments
- the high degree of stress that so many people are under in these waning days of the U.S. empire
- the long-term impacts of infectious diseases, and
- all of the known unknowns in each of these areas — all of the substances that haven’t yet been tested, for instance.
Given all of that: is it really more likely that millions of people are individually subjecting themselves to wildly expensive, supremely taxing medical odysseys and trying to make do on the actual pittance that is social security disability income, just to avoid walking around the block or talking to a therapist once in a while?
Or is something bigger going on?
The deeper you dive into the world of complex chronic diseases, the more the story comes to look like a mirror version of the doubt-and-denial gauntlet that – up until quite recently – surrounded climate change. In both cases, putting the pieces together requires thinking beyond labs and randomized controlled trials, and assembling observational data and models from many sources. It involves listening carefully to the people on the front lines of impact — whether they’re Arctic Indigenous people whose hunting and fishing practices have been disrupted by changes in sea ice, or people who are sick in ways that defy medicine’s present attempt to classify bodies and their ills.
In both cases, the waters have been muddied by powerful actors who are literally invested in keeping on with business as usual. Petrochemical companies came up with individualizing metaphors like “carbon footprint” to get us all arguing about plastic straws while they keep right on drilling in increasingly fragile ecosystems and hiring private armies to assault water protectors. The idea that lifestyle choices drive epidemiological trends might be working in the same way. Maybe that shouldn’t be surprising: in many cases, the same industrial actors are driving both climate change and the inflammatory industrial complex.
In some ways, the needle is starting to move on the matter of complex chronic illnesses: neuro-immune-endocrine interactions, the mediating effects of microbiomes, and the long term impacts of infectious diseases are all rapidly growing areas of research.
But medicine is often slow to change. In the decentralized, largely private U.S. healthcare system, the path from the cutting edge of research to the kind of clinical care that the average American can access is a long, slow trickle. (There’s a reason why the handful of doctors who specialize in treating complex chronic illnesses have waiting lists of a year or more.)
And even if these ideas do eventually become part of mainstream medicine, there’s no guarantee that they won’t be treated just like other diseases presently attributed to “lifestyle” — as something that individuals are responsible for managing themselves through behavior and consumer choices. In fact, this is already underway: check out the marketing copy of “healthy” products or wellness services. Supplements, “nutraceuticals,” and health-conscious food brands are plastered with claims of “anti-inflammatory” and “immune boosting” properties. Online, vaguely credentialled “coaches” claim that they can teach you to “regulate” your nervous system. Probiotics have evolved from yogurt with delightfully mockable commercials (Activia!) to slickly packaged capsules and powders containing carefully calibrated and trademarked selections of bacterial strains, nestled seductively on your favorite influencer’s nightstand.
Cumulatively, it all adds up to the impression that health is a personal achievement — even a vocation. The same sort of thing is visible in the general health advice you find online from major medical institutions. The Mayo Clinic website, for example, warns that stress can “wreak havoc” on the body. But, the article goes on, you should “learn to respond to stress in a healthy way,” because “stress is a part of life” and “you may not be able to change your current situation.” Grand. The mass shootings? The political polarization, the economic instability, the racist and misogynist and anti-queer hostility? Your cartoon villain of a boss? The barely-breathable air and looming threat of power outages, heat waves, fires, storms, and cold snaps that could knock your whole community off its axis overnight? All just a part of life! Not a shared, planetary existential predicament — just your current situation.
Be sure to meditate as the hurricane rolls in.
To be clear: “lifestyle” recommendations aren’t meaningless. For people already experiencing the ill effects of a chronically strained supersystem, reducing exposure to toxins and stressors, avoiding infectious diseases, and eating a diet that doesn’t further aggravate symptoms can make a substantial difference in quality of life. These may be necessary steps to regain what the relatively able-bodied among us would think of as a basic level of functionality — the ability to hold a job, to cook a meal, to spend time with loved ones. Hell, even the ability to get out bed and take a shower. Nutritious food and quality rest (and respite from chemical assault) is no trivial part of healing any disease. These should be things we all have, before we get sick.
Ultimately, as long as the petrochemical refineries exist, some people are going to have to live closer to them than others. As long as ultra-processed, microbiome-destroying, additive-laden foods are the cheapest, someone is going to reach for them. As long as someone’s using the industrial pesticides, they’ll keep running off into the groundwater, the rivers, and the oceans, and falling with the rain onto the fields marked “organic.”
With the Inflammatory Industrial Complex chugging merrily along, all of us have to deal with it, and part of dealing with it means seeing it. Avoidance, enclosure, detox, building yourself a better bubble - it’s a strategy that, by its nature, will never be an option for everyone.
If things keep going the way they’ve been going, it may not be an option for anyone.
Annika Tara is a PhD candidate in Anthropology at Washington University in St. Louis who researches bodies, the ways we know them, and the ways they fall apart. You can follow Annika online at the bad website via @annikataraa and at @annikataraa.bsky.social on the slightly better one.
That's Heat Death, everybody. We'll be back soon with more interviews and musings on past, future, and all the crises in between. If you enjoy our work, don't forget to subscribe! The more paid memberships we have, the more we can afford to commission longer pieces – something we'd like to do a lot more of.





Member discussion